When the federal prison system began expanding access to medications for opioid use disorder (MOUD), pharmacists like Trey Draude stepped up to help lead the effort.

Draude, who is based at a federal Bureau of Prisons (BOP) facility in Butner, North Carolina, oversees MOUD treatments for people in custody and trains other clinicians to do the same. He also headed up the project to get his complex certified as an opioid treatment program so that providers there may administer methadone.
The grim overdose statistics for newly released inmates underscore efforts to get them started on treatment while they are still incarcerated. But it’s not just the numbers that drive Draude; he is moved, too, by the personal stories he hears from his patients.
“I’ve had patients being tearful with me, upset at their current situation but grateful they’re going to be on treatment,” said Draude, who began working in the prison system in 2015 soon after earning his PharmD. “They’re amazed they’re having a conversation with me about treatment and that there is hope of a change on the horizon.”
Congress directed the BOP to expand MOUD access in its facilities as part of the 2018 First Step Act, a wide-ranging prison reform measure that came amid historic spikes in overdoses, both in communities and correctional facilities. An estimated 15-20% of the federal prison population — which currently stands at 158,000 — has an opioid use disorder.
Today, BOP offers all FDA-approved medications for OUD in its 97 locations. Nearly 12,200 patients have received some form of MOUD, with the vast majority (more than 10,200) receiving buprenorphine, according to officials.
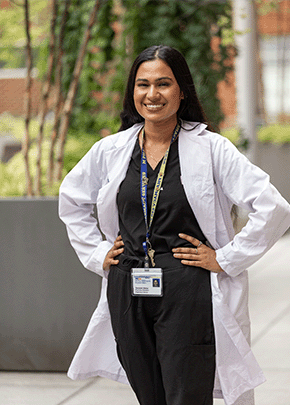
BOP has a long way to go to meet the extraordinary demand. Tami Rodriguez, the system’s director of pharmacy programs and a captain in the United States Public Health Service, said she believes her team will continue making headway, especially with pharmacists championing the effort. Currently, more than 40 BOP pharmacists have collaborative practice agreements that allow them to prescribe buprenorphine.
“When there’s a big project, with a lot of details, pharmacy gets it done,” said Rodriguez, citing the workforce’s leadership on COVID-19 vaccination rollouts and on electronic health record implementation. “I think it’s a culture of pharmacy being reliable and willing to help.”
Early efforts by the BOP to provide MOUD treatment got off to a slow start due to pandemic restrictions and such bureaucratic hurdles as the federal X-waiver, which required extensive training for some providers and prohibited others, including pharmacists, from even prescribing buprenorphine, according to Rodriguez.
ASHP helped lead the successful fight to eliminate the X-waiver requirement. Even though the federal restriction is now gone, only 10 states allow pharmacists to initiate such treatments. ASHP last year released model state legislation to allow pharmacists to prescribe MOUD.
ASHP has also created one of the nation’s few MOUD training programs geared toward pharmacists and any other providers ready to lead this treatment. The program meets federal training requirements for the Medication Access and Training Expansion Act of 2023.
Like the Veterans Administration’s clinical pharmacist practitioners, BOP pharmacists are authorized to initiate, adjust, and discontinue medications under collaborative practice agreements and were poised to begin managing buprenorphine for OUD once the X-waiver was lifted.
But BOP didn’t have to contend just with bureaucracy before it could begin implementing MOUD. It also had to undergo a dramatic cultural shift, Rodriguez noted. Before 2018, the system provided only abstinence-based services for most patients with OUD. And like all correctional facilities, the BOP deals with contraband, including easy-to-conceal buprenorphine/naloxone strips, making its way to the prison population, she said.
“We’ve had this culture of abstinence-based treatment for substance use disorders and doing everything we can to keep illicit substances out of our system,” she said. “So that’s been a huge change in mindset.”
That goes not just for employees, but also for inmates who participate in substance use disorder behavioral therapy programs. Those programs focus on accountability, and she said there may be a perception that fellow patients who are receiving MOUD “don’t really want to be clean.”

Fighting such perceptions is a significant part of her team’s educational efforts. A critical starting point, said Josh Valgardson, chief of the BOP’s clinical pharmacy program, is recognizing that opioid use disorder is a chronic condition, like diabetes.
“Our pharmacists have really stepped up to help with chronic disease state management,” Valgardson said. “Opioid use disorder is no different.”
BOP clinicians must plan for what happens once their patients leave. “The first day we see them we have to be thinking about how they’re going to access treatment once they get out,” said Rodriguez.
“The last thing we want to do is start a patient on methadone and then release them and they aren’t able to continue it. Or try to change them to buprenorphine a month before they leave, while they’re struggling with all the challenges of planning for reentry to their community.”
In Butner, Draude said the demand for MOUD outpaces the ability to provide it. “Sometimes they’ll see me and plead their cases as to why they should be next in line,” he said.
When the facility began offering the medications in 2019, it prioritized the men who were leaving prison and moving into halfway houses that offered medications.
Currently, Butner prioritizes MOUD for patients whose release date is within a year. However, as the capacity to provide MOUD continues to expand, Butner and the BOP’s goal is to provide the treatment to every patient when clinically indicated.
Often patients are unwilling to admit to drug use due to concerns of disciplinary action. Draude reminds the patients who see him for MOUD that his priority is helping them receive the care they need. “It’s a medical setting, and information they share regarding their opioid use disorder is confidential,” he said. “The medical labs I order are not used against them in any disciplinary process. They usually are comfortable at that point to have a conversation.”
BOP does not yet have outcomes data for its expansion of MOUD but recently hired an epidemiologist, who will lead data collection for a study. System-wide, the BOP is expanding its capacity to treat OUD by expanding its telehealth program so that short-staffed institutions will have additional support via telehealth, said Rodriguez. Initially, the telehealth program started with physicians, with plans to add pharmacists in the future.
“I think the federal Bureau of Prisons could provide a great model of what states can do if they allow pharmacists to practice in the same way that our pharmacists do,” Rodriguez said.